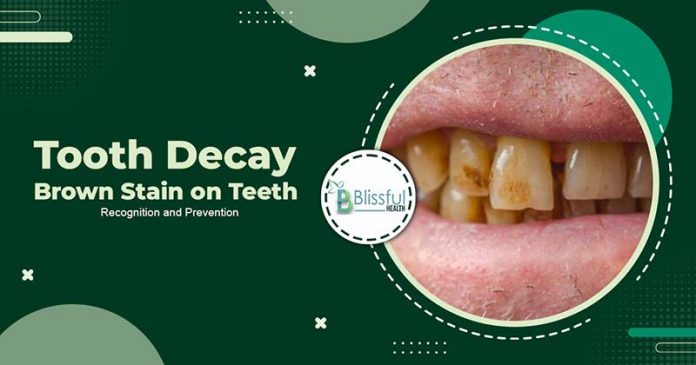
Brown tooth decay, often marked by discoloration spots on the teeth, can vary widely in appearance. These spots, ranging from yellowish-brown to black-brown, may present as irregular patches or defined brown lines.
At Blissfulhealth, we delve into “Tooth Decay Brown Stain on Teeth,” examining the causes and discussing effective prevention and removal strategies. By adopting targeted lifestyle changes and considering professional dental treatments, individuals can combat this common dental issue.
Join us as we explore how to maintain your dental health and restore the natural beauty of your smile.
Recognizing Brown Spots and Tooth Decay on Teeth
Brown spots on teeth can stem from various factors, such as inadequate oral care, smoking, tooth decay, aging, fluorosis, enamel hypoplasia, root canal problems, injuries, previous dental procedures, medications, and certain health conditions like celiac disease. These spots can vary in color and appearance, ranging from patchy discoloration to lines, and might signal underlying health issues.
Tooth decay, tartar accumulation, fluorosis, enamel hypoplasia, injuries, and past dental treatments commonly cause brown spots on teeth. Maintaining good oral hygiene, regular dental check-ups, and seeking appropriate treatment are crucial for addressing brown spots and preventing further dental complications.

Causes of Brown Spots on Teeth
Brown spots on teeth can be attributed to a variety of factors:
Foods and Drinks:
Dark-colored foods and beverages contain compounds known as chromogens, which have the potential to stain tooth enamel over time. For instance, red wine contains tannic acid, which contributes to staining.
If oral hygiene is lacking, these stains may become more entrenched. Furthermore, foods and drinks with artificial colors and dyes can also lead to significant staining of the teeth.

Nicotine and Tobacco Products:
Particles present in tobacco and nicotine products can adhere to the microscopic pores found in tooth enamel. With repeated use, these particles accumulate, leading to the gradual darkening of teeth. Over time, these stains tend to become more stubborn and challenging to remove.

Tartar Formation:
The mouth hosts thousands of bacteria that, when combined with saliva and food remnants, form a sticky, translucent film called plaque. Effective oral hygiene practices such as brushing and flossing help control plaque levels.
However, inadequate oral care can result in plaque hardening into a more permanent substance known as tartar or calculus. Once tartar has formed, only dental professionals can remove it. Factors such as smoking, illness, diabetes, hormonal fluctuations (such as those during puberty, pregnancy, and menopause), and certain medications can heighten the risk of tartar buildup.
Tooth Decay:
Bacteria present in plaque and tartar feed on sugars in the mouth, producing acids that erode enamel. The persistent presence of these acids on the teeth can lead to the exposure of the yellowish layers of tooth beneath, resulting in yellowish-brown discoloration.
In cases of severe decay, acids may create cavities within the tooth, which appear darkly colored. Even minor cracks or breaks in teeth can provide entry points for bacteria, leading to decay. It’s common for individuals to develop dark spots of decay around the edges of dental fillings or crowns if bacteria enter through crevices. Dental cavities can cause discomfort and sensitivity to hot or cold foods and beverages, particularly when they expose the tooth’s root or nerve.
Aging:
With age, the protective white enamel covering the teeth gradually deteriorates, revealing the yellow dentin layers beneath. This natural aging process can result in the appearance of yellowish-brown spots or large patches of discoloration on the teeth.
Genetics:
The natural color of an individual’s teeth varies, influenced by genetic factors. Genetic predispositions can affect the strength of tooth enamel, its response to pigments and acids, and the degree of wear and tear it experiences.
Hereditary conditions such as dentinogenesis imperfecta and developmental disorders affecting bone and tooth formation can also influence tooth color and structure.
Previous Dental Work:
Dental restorations such as fillings, crowns, and bridges may degrade over time, causing them to lose their color or transfer metal color into the surrounding tooth structure.

Medications:
Certain medications, notably the antibiotic tetracycline and its derivatives, can cause tooth discoloration, particularly in young children. Other medications associated with brown spots on teeth include glibenclamide (Glynase) and chlorhexidine, a medicated mouthwash.
Enamel Hypoplasia:
Enamel hypoplasia results from developmental disruptions that cause enamel to be thin but hard. Affected teeth may exhibit chalky white or yellowish-brown patches.
Causes and risk factors for enamel hypoplasia include inadequate nutrient intake (especially calcium), birth injuries or premature birth, viral and bacterial infections (such as measles or chickenpox), maternal illness or malnutrition during pregnancy, exposure to toxins and allergens, fluoride ingestion (fluorosis), tooth injuries, or damage.
Celiac Disease:
Dental symptoms often serve as early indicators of celiac disease, manifesting as patches or speckles of brown, yellow, or whitish discoloration, weak enamel, pitting, and translucence. These issues typically affect the molars and incisors on both sides of the mouth.
Fluorosis:
Excessive fluoride intake, particularly in children under the age of 8, can result in enamel staining. This condition, known as fluorosis, may present as white or greyish streaks across the teeth, and in severe cases, dark brown spots and pits. Although fluorosis symptoms may resemble those of tooth decay, the condition is generally benign.
Treatment Options for Brown Spots on Teeth
The appropriate treatment for brown spots on teeth depends on their underlying cause. Here are some options:
Home Remedies: For stains caused by foods, beverages, or lifestyle habits like smoking, several home remedies can be effective:
- Brushing with a mixture of baking soda and water every few days.
- Rinsing the mouth with a diluted hydrogen peroxide solution daily or every few days, followed by rinsing with water.
Over-the-Counter Products: Various over-the-counter products can help eliminate tooth discoloration. Results typically appear within 1–2 weeks, but outcomes may vary:
- Whitening mouthwashes and rinses containing hydrogen peroxide.
- Whitening toothpastes with sodium hypochlorite.
- Whitening strips containing carbamide peroxide.
- Tray whitening systems featuring carbamide peroxide bleaching gel.

Professional Dental Treatment: If discoloration stems from tartar buildup or medical conditions, a dental visit may be necessary. Dental professionals can:
- Use specialized instruments to remove tartar and plaque from teeth.
- Perform minor procedures like bleaching and topical fluoride application to whiten teeth and prevent further decay.
Permanent Discoloration: Certain types of tooth discoloration, such as those related to celiac disease, fluorosis, or severe decay, may be permanent. In such cases, a dentist can consider the following options to address or conceal stubborn discoloration:
- White composite fillings.
- Veneers.
- Crown.
Additionally, wearing a night guard or retainer may be recommended to prevent further discoloration or damage.
Consulting a dentist is crucial for determining the most suitable treatment based on individual needs and the specific cause of tooth discoloration.
Prevention Tips for Tooth Decay Brown Stains on Teeth
Maintaining good oral hygiene is key to preventing brown spots on teeth. Here are some helpful tips:
- Brushing: Brush your teeth with fluoride toothpaste for 2 minutes, twice daily.
- Flossing: Floss daily to remove plaque and food particles from between teeth.
- Rinse or Brush After Eating: Rinse your mouth with water or brush your teeth after consuming meals, especially if they’re high in sugar, chromogens, or tannins.
- Fluoride Mouthwash: Use a fluoride-based mouthwash daily (not recommended for children under 6).
- Regular Dental Check-ups: Schedule regular dental cleanings and assessments to detect and address any early signs of discoloration or decay.
- Quit Smoking: Stop using nicotine or tobacco products to prevent staining and maintain oral health.
- Use a Straw: When drinking beverages other than water, use a straw to minimize contact with teeth.
- Address Teeth Grinding: Talk to your dentist about habits like teeth grinding that may harm your teeth and explore possible solutions.
- Avoid Staining Agents: Certain foods and beverages can stain teeth and weaken enamel. It’s advisable to limit or avoid:
- Sugary foods and drinks.
- Foods with artificial coloring.
- Coffee, tea, red wine, and dark liquors.
- Dark fruit juices and citrus fruits and juices.
- Dark sauces like soy sauce and tomato sauce.
- Choose Enamel-Strengthening Foods: Some foods can help strengthen enamel and prevent discoloration by scrubbing away bacteria and plaque or neutralizing acids. Consider incorporating these into your diet:
- Green, leafy vegetables like kale, spinach, and broccoli.
- Cheeses and fermented yogurts.
- High-fiber fruits and vegetables such as apples, plums, pears, and celery.
- Foods rich in antioxidants like carrots, ginger, and garlic.
- Whole grains and cereals.
FAQ
Is a brown tooth indicative of a cavity?
Yes, a brown tooth can indicate a cavity. Tooth decay can progress to form a cavity, with brown or black discoloration being a visible sign. This discoloration results from enamel and dentin destruction, stained by the decay process.
Can a tooth with brown stains be saved?
Yes, a tooth with brown stains can often be saved depending on the cause and extent of discoloration. If caused by a cavity, treatments like fillings, crowns, or root canals may be necessary. Superficial stains from foods, beverages, or smoking can be treated with professional cleaning and whitening treatments.
Do genetics influence brown stains on teeth?
Genetics can influence susceptibility to dental conditions leading to brown stains. Some individuals may have genetically weaker enamel, making teeth more prone to decay and staining.
Genetic conditions affecting enamel and dentin development can also cause discoloration. However, environmental factors like diet and oral hygiene are typically more influential in causing brown stains.
Conclusion
In conclusion, the primary factors leading to “Tooth Decay Brown Stain on Teeth” include poor dental hygiene, smoking, or frequent consumption of dark-colored foods and beverages. These external discolorations are generally preventable and treatable with good oral care practices. However, persistent brown spots may sometimes signal underlying health issues or side effects from medications.
If over-the-counter treatments do not clear these spots, or if they are accompanied by other symptoms, it is crucial to seek professional advice. A consultation with a dentist or healthcare provider is advisable to properly address the causes of tooth discoloration.